I must admit, I’m a big picture person-statistics has never been one of my favorite subjects but the COVID pandemic is certainly challenging me (and all of us) to pay attention to epidemiology and statistics! I’ve also learned over the years as a physician to take medical testing in to account and use the results in context. I recall, while in residency, I felt a pelvic mass on a patient but the CT scan was read as normal. I trusted my instinct and challenged this and when the scan was re-read they discovered a mass of the bladder!
I’ve been trying to more fully understand the evolving situation of COVID19 testing- here in Austin particularly- as I want to apply testing and advise patients appropriately. I wish we had better testing. As a physician I have grown to rely on my training and gut instinct for recognizing patterns -but there is more at risk with this virus and I wouldn’t want to misdiagnose COVID as say, a sinus infection. In fact, my first patient that had a positive swab through Austin Public Health had presented to me with concerns about having a bad sinus infection.
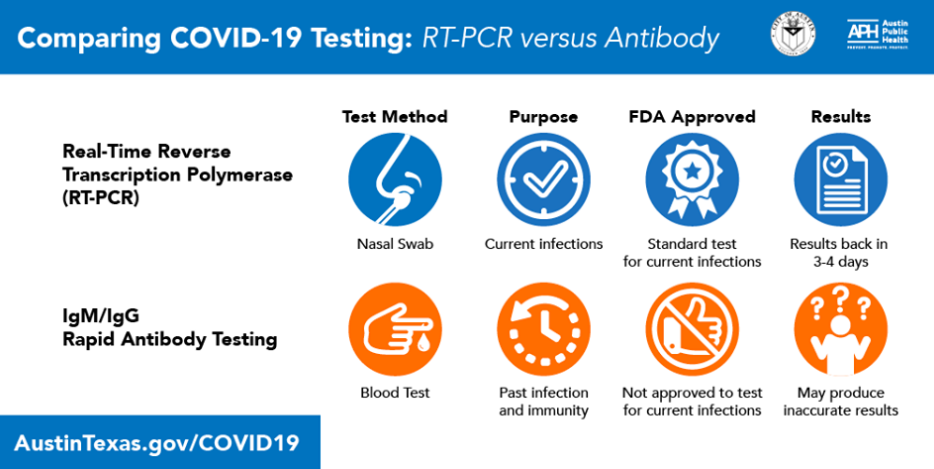
Navigating the ever evolving information about testing can be difficult, so I wanted to explain simply as I understand thus far. COVID19 Testing can answer two questions: Do I have the COVID19 virus? -OR- Did I have the COVID19 virus? Within each of these questions, there is a myriad of other statistical presumptions that impact sensitivity and specificity, as well as false negative and false positive results- but that is beyond the scope of this blog.
I wanted to provide you with the basics:
Question 1: Do I have the COVID19 virus?
Test Needed: nasal/pharyngeal swab/ PCR test
This is available through Austin Public Health and other sites, such as hospitals. (PCR tests for the viral RNA). The normal turnaround time now is 24-72 hours. You may have heard in the news about an Abbott Test that also checks a nasal/pharyngeal swab and has a 5-15 min turnaround time but it is not widely available at this time. Walgreens may be offering it soon locally. As of now, the swab that goes into your nose and up to your sinuses, that you have to wait at least a day for results, is the only way to get results of active COVID as an outpatient.
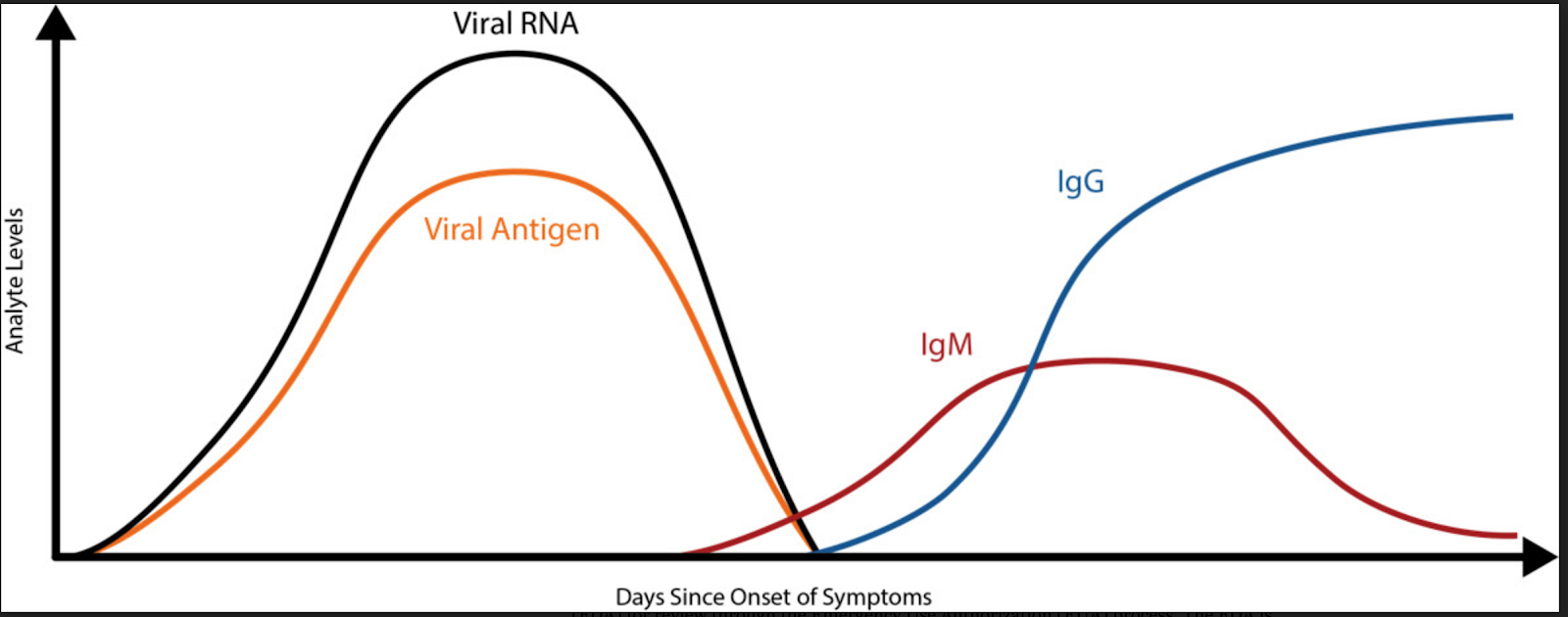
From what I can tell, it will be more accurate if the virus is actually shedding in your nasal cavity. It may be most accurate about 7 days into experiencing symptoms and it could be missed if completed too early or too late. I have also read that this test has a 1 in 20 chance for being inaccurate.
DID I have the COVID19 virus?
Test Needed: blood test: finger prick or blood draw from arm
Beware of when during your illness you get this test AND how these results are interpreted. These tests vary greatly in accuracy.
These tests are called serological tests. They are in the news and now at various clinics around town. They are very appealing because of the fast turn around time and wide availability.
The CDC reports “Data that will inform serologic testing guidance is rapidly evolving. Recommendations on the use of serologic tests to determine protective immunity and infectiousness among persons recently infected with SAR-CoV-2 will be updated as new information becomes available.”
Serological tests measure the amount of antibodies or proteins present in the blood when the body is responding to a specific infection, like COVID-19. In other words, the test detects the body’s immune response to the infection caused by the virus rather than detecting the virus itself. In the early days of an infection when the body’s immune response is still building, antibodies may not be detected. This limits the test’s effectiveness for diagnosing COVID-19 and why it should not be used as the sole basis to diagnose COVID-19.
I use other IgM and IgG tests all the time in my medical practice. Having IgM elevated shows a more acute infection and IgG shows a past infection. So they can help us get information about your immune response but not the acute presence of a virus or infection.
We stand with Austin Public Health on antibody testing, they advise: “At this time, we do NOT recommend taking these tests, even those with EUAs, until further evaluation of them has been done. Even if they are accurate, what to do with that information is up for debate. At this point, they are a waste of your money, and worse, may cause you to alter behavior that would otherwise protect you.”
- The majority of these tests have not been reviewed by the FDA.
Negative results do not rule out SARS-CoV-2 infection, particularly in those who have been in contact with the virus. - Follow-up testing with a molecular diagnostic should be considered to rule out infection in these individuals.
- Results from antibody testing should not be used as the sole basis to diagnose or exclude SARS-CoV-2 infection or to inform infection status.
- Positive results may be due to past or present infection with non-SARS-CoV-2 coronavirus strains, such as coronavirus HKU1, NL63, OC43, or 229E.
So, to be clear, These tests are NOT accurate for detection of acute illness.
While data at this point is still limited, it appears that the initial IgM antibody response does not peak until roughly 9 days after initial infection, and the IgG antibody response does not peak until around day 11.
In March, in order to speed up test availability, the FDA issued a policy to allow developers to market their tests that meet certain criterias without prior FDA review. The FDA to date has only authorized ONE serological test for COVID19 that is intended for use by clinical laboratories. Be wary of companies offering “at home, FDA Approved” testing.
Since these serology tests have not gone through the normal comprehensive FDA approval process, some may have more statistical limitations and may not be as accurate. For example, these tests detect an antibody that is formed in response to the common cold coronavirus not COVID19.
Serological tests likely will play a critical role in the fight against COVID-19 by helping healthcare professionals learn about individuals who have overcome the infection and developed an immune response. In the future, this may potentially be used to help determine, together with other clinical data, that such individuals are no longer susceptible to infection and can return to work. In addition, these test results can aid in determining who may donate a part of their blood called convalescent plasma, which may serve as a possible treatment for those who are seriously ill from COVID-19.
We still have much to learn about the ability and application of COVID19 testing & results. This testing will be imperative for us to be able to start moving around more. Thank you all for following the physical distancing and safety recommendations while they continue to sort out testing.
In summary, thus far COVID19 tests can help us understand (1) if a person is infected with COVID19 (2) if a person has been previously infected with COVID19, given that the test is performed within a certain time period.
- If you suspect you have COVID19 symptoms, reach out to your healthcare provider or call 211. We are also available via telemedicine.
- If you do a blood test early on, please don’t assume that being negative is the end all.
- If you did a nasal swab and resulted negative but still have symptoms, please continue to isolate and keep in close touch with your medical provider.
- Don’t rush to do the blood testing: From observation, the cytokine “storm” occurs around 10 days after symptoms start- which is around the time serum (blood) antibodies peak, so blood testing is not to detect acute illness but rather for tracking and epidemiology. Austin Public Health is unveiling a public facing testing platform for people to get direct access PCR testing that is said to be released later this week.
- Stay up to date with latest information on your local state and city websites, as well as cdc.gov and who.int
Stay safe & healthy. Thank you all for your patience as we continue to fight this battle! We are here for you!
*This information is based on our understanding as of April 16, 2020 and is subject to change
updated May 11, 2020
Resources/ Sources:
Interpreting COVID19 Testing
COVID19 Public Testing Enrollment
Austin Travis County: COVID19 resources
APH on testing
FDA on Serologic (blood) testing
FDA’s EUA (Emergency Use Authorizations)
CDC Priority COVID testing
Why we need Antigen & Antibody tests for COVID19
False Negative concerns- COVID19 testing
Walgreens COVID19 FAQs
Why You Can’t Always Trust Your Coronavirus Antibody Test Results
“Austin & Travis County Public Safety Joint Statement on COVID19 Antibody” Testing
Interim Guidelines for COVID-19 Antibody Testing